Laureate Professor Clare Collins AO in Nutrition and Dietetics at the University of Newcastle, emphasises the need for accurate and reliable nutrition information to reach the public. Prof Collins believes that it is vital for clinicians to stay up-to-date with cutting-edge nutrition science and work with communication organisations to disseminate information to the general public. This is particularly important as social media is full of both reliable and unreliable information on dietary patterns, such as veganism.
Prof Collins notes that there are health risks associated with veganism and advises that people should approach it with caution. Iron, iodine, and bone density should be checked regularly for those who follow a vegan diet.
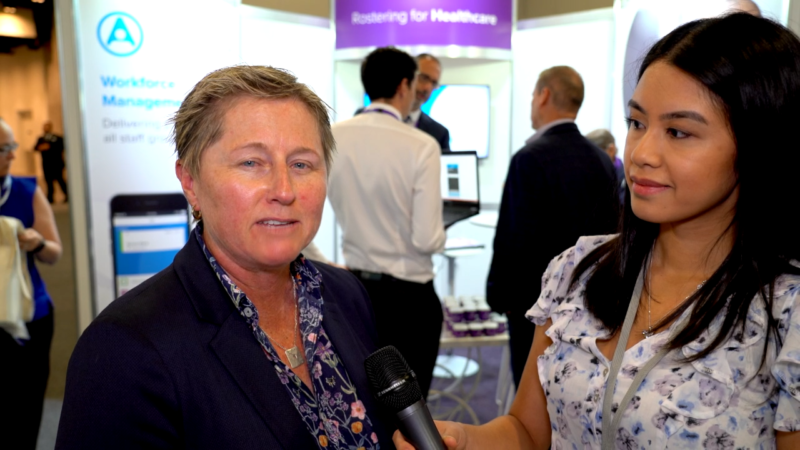
In an interview with Australian Health Journal, Professor Collins suggests that clinicians should counter misinformation on social media and stay up-to-date with the latest nutrition science to provide evidence-based advice to their patients. Regular check-ins with patients are also essential to evaluate their dietary patterns and address any nutritional deficiencies.
It is important for healthcare professionals to understand the risks and benefits associated with patient engagement to ensure that patients remain engaged in their healthcare. By doing so, patients are more likely to stay committed to their healthcare journey instead of feeling unheard and walking away from their healthcare provider.
It’s also crucial for healthcare professionals to be aware of high-level marketing activities that promote unhealthy foods and supplements in the food supply. The supplement market is worth billions of dollars, and many of the supplements available on the market are unnecessary for the general population, according to Prof Collins.
While certain supplements may be necessary for specific health conditions, the majority of supplements have no scientific evidence to support their effectiveness. Therefore, healthcare professionals should be cautious and skeptical about the need for supplements and also stay informed about what’s being marketed to patients for conditions such as pain or arthritis. Additionally, it’s essential to recognise that many food products are driven by big food companies, who stand to profit from people becoming addicted to their food products.
Above all, health care professionals need to know where to direct people to evidence-based information. Globally, people can access information via The Conversation, a free public website that is a collaboration between academics and journalists to translate evidence-based information into readable, practical, and usable advice.
In her research, Prof Collins created a website called “No Money, No Time,” where nutrition research evidence is synthesised into bite-sized short reads and linked to recipes so that people can use nutrition science. This way, people do not have to wait for years for the translation of advice on what to eat for health.
Professor Clare Collins is a dietitian with over 40 years of experience, currently holding an NHMRC Level 3 Leadership Research Fellowship and a Fellow of Dietitians Australia. In the past and in her career, assessing someone’s nutrient intake was a time-consuming task that required collecting a detailed diet history and manually calculating nutrient contents. However, in recent research, Prof Collins has developed cutting-edge tools that can analyse dietary intake and provide detailed information in as little as 15 minutes.
Prof Collins believes that the future of nutrition science lies in precision and personalised nutrition, which takes into account an individual’s genetics, nutrient requirements, and response to dietary interventions. Her research also explores the relationship between technology tools and biomarkers found in blood or urine, and how these tools can be integrated into primary care to improve nutrition-related healthcare for all.
You Might also like
-
Upskilling & empowering Health Professionals to support preconception to pre-school level health
A new podcast series, developed by Health and Wellbeing Queensland, is designed to upskill and empower health professionals in their support of parents from preconception through to the pre-school years.
Clinician’s Guide to the First 2000 Days follows the success of Health and Wellbeing Queensland’s first podcast series Clinician’s Guide to Healthy Kids, launched in 2023. Both focus on supporting health professionals to have effective conversations on positive health behaviours.
-
Michelle Fenwick – Northern Health
The outskirts of Melbourne is experiencing significant population growth over the next 10 years and Northern Health has taken preemptive steps to ensure the supply of new talented healthcare staff as well as develop the culture of the workplace.
Michelle Fenwick, the Executive Director of Northern Health spoke with our reporter Anne Dao on the challenges of this urban growth over the past 3 years. By 2031 the region is expected to increase in population by 63%. Added to this is hiring and training the right workforce to align with the clinical care needs of people coming into the healthcare centres.
Culture is forming in a growing organisation with approximately 70% of staff having been at Northern Health less than 4 years. However there is opportunity for clinical staff to accelerate their career in such an environment
Post Views:
2,333 -
Rural allied health mentorship program creates opportunities for students and practice
Melanie Roll, a director and physiotherapist at Gen Health Hamilton, is dedicated to nurturing the next generation of allied health professionals. Gen Health’s support begins with a work experience program for local secondary school students, where they can observe a variety of health services and participate in an annual careers night to explore allied health career pathways.
Upon moving to tertiary education, students are offered placements through a five-week program designed to transition them from observation to supervised practice and ultimately to seeing their own patients. In their final study year, they can apply for the mentorship program, which aids the transition into private practice.