IMPERATIVE NEED TO IMPROVE OUTCOMES FOR WOMEN DIAGNOSED WITH OVARIAN CANCER. ANZGOG Chair gives stark assessment on late diagnosis, limited treatment options and significantly low survival rates
With
Professor Clare Scott, Chair
Australia New Zealand Gynaecological Oncology Group (ANZGOG) &
Clinician Scientist
WEHI The Walter and Eliza Hall Institute of Medical Research &
Medical Oncologist, Peter MacCallum Cancer Centre, The Royal Women’s Hospital and The Royal Melbourne Hospital
Australian Health Journal Talk
Filmed Online | April 2025
Professor Clare Scott, a pioneering clinician scientist at the Walter and Eliza Hall Institute of Medical Research in Melbourne, also serves as a medical oncologist at Peter MacCallum Cancer Centre, the Royal Melbourne Hospital, and the Royal Women’s Hospital.
Her comprehensive training in medical oncology has fuelled her specialisation in gynaecological cancer, combining rigorous research with clinical trials to improve patient outcomes. With over a decade of involvement in ANZGOG, Australia’s foremost gynaecologic cancer research organisation, she is deeply committed to advancing research and saving lives.
ANZGOG’s values—excellence, impact, equity, collaboration, and openness—reflect the organisation’s dedication to transformative cancer research. Its strategic plan is designed around four comprehensive goals, aiming to initiate innovative, practice-changing gynaecological cancer research. This not only expands the reach of impactful studies but also ensures that research directly benefits the community, ultimately improving the lives of countless women affected by these cancers.
Ovarian cancer, a complex and diverse group of diseases, poses significant challenges in diagnosis and treatment. While high-grade serous ovarian cancer is often highlighted, other rare types also demand critical attention. With projections indicating over 1,800 Australian women will be diagnosed by 2025, and a startling survival rate of just under 50%, Professor Scott talks of the need to rally together to confront this pressing public health issue. Tragically, two-thirds of cases are diagnosed at an advanced stage, diminishing survival prospects further. As of now, around 5,300 Australian women live with ovarian cancer, facing ongoing challenges that necessitate urgent action and support.
In this Australian Health Journal Talk, Professor Scott talks in detail about the following –
- The incidence of ovarian cancer in Australian women and mortality statistics around advanced stage diagnosis
- The symptoms and why they get dismissed or misdiagnosed
- The challenges in access to screening, treatment and funding for research
She also delivers a message to the medical community and the Australian Government.
Source: Generative AI on transcript
You Might also like
-
Australian Primary Health Care Nurses Association Career Federal Budget General Practice New Content Nursing
A New Era in Primary Health Care Nursing
Coinciding with this year’s International Nurses Day, this week’s Federal Budget has had some significant outcomes for the primary health care, nursing workforce.
The Federal Budget delivered on 9th May 2023, APNA believes will strengthen Australia’s primary health care (PHC) system by addressing growing nursing shortages, seeing more nurses hired where they are needed, and better utilising the largest workforce in PHC of nearly 100,000 nurses to their full potential to reduce the pressure on the health system.
-
1 million Australians with undiagnosed thyroid disorders remain at risk of irreparable damage
The Australian Thyroid Foundation is a national not-for-profit organisation with charity status aimed at patients and the healthcare community. The ATF’s focus is to support and educate its member base and promote our Good Thyroid Health Messaging throughout the Australian Community.
Australian Thyroid Foundation, CEO Beverley Garside attending the breakfast gave her response to the Federal Budget and the Foundation’s pre-budget submission, which was not granted.
-
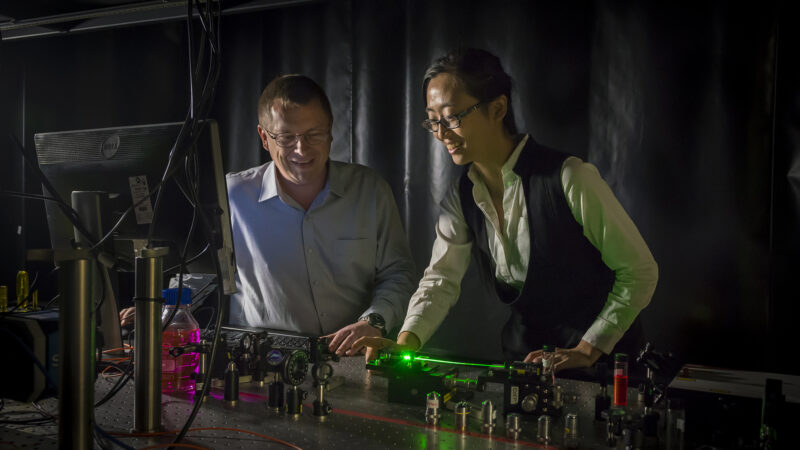
Hair’s-breadth endoscopes to detect plaque
This coming World Heart Day (29th September 2021), Australian Health Journal’s People in Health Care series, releases a segment on Dr Jiawen Li.
Dr Jiawen Li is an inventor and highly adaptable engineer leading the intravascular imaging program at the Institute of Photonics and Advanced Sensing (IPAS). She has developing an imaging device can be inserted into blood vessels to provide high quality 3D images to help scientists better understand the causes of heart attack and heart disease progression, and could lead to improved treatment and prevention.