Communities across Australia rely on Registered Nurses (RNs) to provide primary care, acute care and aged care. They are skilled, capable and trusted healthcare practitioners often working in some of the most rural and remote parts of the country.
In March 2023, the Australian Government released the National Rural and Remote Nursing Generalist Framework 2023–2027. The Framework is a world first and describes the unique context of practice and core capabilities for rural and remote Registered Nurses in Australia.
As well as describing skills, capabilities and support needed by RNs, the Framework emphasises the importance of clinical decision-making judgement of the patient’s situation, culturally safe practice, collaboration, and partnerships with clients, families and communities.
The framework is for RNs who work in rural and remote locations across Australia, or are looking to relocate there. One such nurse who relocated is Clinton Archer, with Queensland Health, who was interviewed by Australian Health Journal for this segment.
Other ways the the Framework can be applied include:
- For Registered Nurses, mapping their development of the capabilities with a mentor, to develop from formative to proficient skill levels.
- For Educators and Education Providers, supporting individual skill development or curriculum based on the capabilities.
- Government, Organisations and Employers, using the Framework as a guide to grow and support the development of a skilled rural and remote RN workforce
The Framework was developed by the Office of the National Rural Health Commissioner and Australian Health Journal spoke with National Rural Health Commissioner, Adjunct Professor Ruth Stewart, and Deputy National Rural Health Commissioner – Nursing and Midwifery, Adjunct Professor Shelley Nowlan, on the importance of rural and remote nursing and of the Framework itself.
Important contributions and expertise of the members of the National Rural and Remote Nursing Generalist Framework Steering Committee (Steering Committee) led the Framework through its development and consultation. Steering Committee members represented the following organisations.
- Office of the National Rural Health Commissioner
- Australian Government Department of Health and Aged Care
- Australian and New Zealand Council of Chief Nursing and Midwifery Officers
- Australian College of Nurse Practitioners (ACNP)
- Australian College of Nursing (ACN)
- Australian Nursing and Midwifery Accreditation Council (ANMAC)
- Australian Nursing and Midwifery Federation (ANMF)
- Australian Primary Health Care Nurses Association (APNA)
- Congress of Aboriginal and Torres Strait Islander Nurses and Midwives (CATSINaM)
- Council of Deans of Nursing and Midwifery (CDNM)
- Council of Remote Area Nurses of Australia (CRANAplus)
- James Cook University
- Nursing and Midwifery Board of Australia (NMBA)
You Might also like
-
Michelle Fenwick – Northern Health
The outskirts of Melbourne is experiencing significant population growth over the next 10 years and Northern Health has taken preemptive steps to ensure the supply of new talented healthcare staff as well as develop the culture of the workplace.
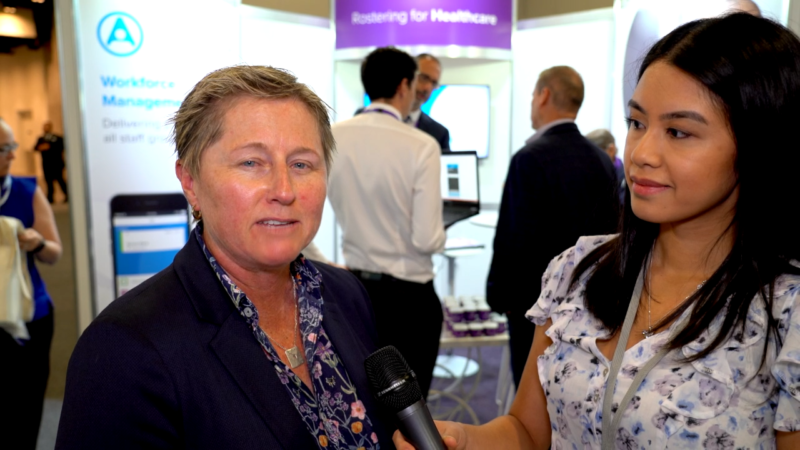
Michelle Fenwick, the Executive Director of Northern Health spoke with our reporter Anne Dao on the challenges of this urban growth over the past 3 years. By 2031 the region is expected to increase in population by 63%. Added to this is hiring and training the right workforce to align with the clinical care needs of people coming into the healthcare centres.
Culture is forming in a growing organisation with approximately 70% of staff having been at Northern Health less than 4 years. However there is opportunity for clinical staff to accelerate their career in such an environment
Post Views:
967 -
Child Dental Benefits Schedule needing greater awareness
Since its launch in 2014, the Child Dental Benefits Schedule has seen a gradual increase in participation year on year. The impact of COVID-19 and related shutdowns saw participation fall sharply in 2020. Though it increased 2021, the national target of 41% participation was not reached in 2021-2022, with the total (35.4%) more than three percent below 2018 participation rates.
In an opinion segment, Australian Health Journal spoke with Abano Healthcare Group Clinical Director, Dr Fred Calavassy, with over 30 years of clinical experience, about his observations of the Child Dental Benefits Scheme ways to increasing participation rates.
-
Values in Workplace Culture
Professor Sabe Sabesan, is the Clinical Dean of the Townsville Regional Medical Training network incorporating the Townsville Hospital and Health Services and the Townsville Clinical School of the James Cook University and the director of the department of Medical oncology at the Townsville Cancer Centre, Townsville Hospital.
The Professor recently wrote, “Workforce wellness and engagement have become buzzwords in healthcare settings since there is an intimate relationship between staff wellbeing and performance of the healthcare system. Wellness initiatives such as wellness champions and wellness committees have been set up in response to emerging workforce mental health issues. These are largely reactive rather than being proactive in addressing or preventing the root cause of mental health issues.”