Next week, at the Perth Convention and Exhibition Centre, The Royal Australian and New Zealand College of Psychiatrists (RANZCP) meet for the RANZCP 2023 Congress on the theme of “New Horizons: Connected Futures”
Delegates have been invited to reflect on how interconnectedness is a strength; and connections with each other in personal and professional lives, connections with the diverse cultures in communities, and connection to place with First Nations people.
Looking forward delegates have been asked to consider the next horizon in biological psychiatry and the delivery of evidence-based treatments. They have been asked to consider how the criminal justice system, mental healthcare system, disability sector and drug and alcohol services are interwoven and how to provide care that is integrated, and person centred.
Australian Health Journal spoke to current President-Elect Dr Elizabeth Moore and soon to be President, RANZCP about the Congress, as well as the recent Federal Budget announcements around mental health funding.
The RANZCP has welcomed a number of measures:
- $260.2 million over two years from 2023–24 to extend Commonwealth psychosocial supports for people with severe mental illness who are not in the National Disability Insurance Scheme (NDIS)
- $0.9 million over two years from 2022–23 to develop a 10 Year National Action Plan to support the health and wellbeing of Lesbian, Gay, Bisexual, Transgender, Intersex, Queer and Asexual (LGBTIQA+) people and establish a LGBTIQA+ Health Advisory Group.
- $40.0 million over 4 years from 2023–24 to establish the National Clinical Quality Registry Program for tracking the safety and performance of treatments and devices, thereby improving performance reporting for clinicians and hospitals.
- $4.9 billion over 5 years from 2022–23 (with $1.3 billion per year ongoing) to increase support for people receiving working age payments including the JobSeeker Payment. As noted in the College’s submission to the Senate Inquiry into poverty in Australia, we urged for an increase to the allowance rate for Australians accessing government-funded payments, including JobSeeker.
However, while there are some positive measures for mental health, RANZCP believe funding has been weighted to wellbeing initiatives and primary care. Australians experiencing the most serious mental health conditions, with severe, complex and chronic presentations have missed out on vital support in this year’s Federal Budget.
A particular group of concern is children. Around 3 in 4 children with a severe mental health disorder are missing out on critical support, according to Dr Moore.
Out of the 80,000 children in Australian with a severe mental health condition, only 22,000 are currently being seen by a psychiatrist, stating the case that more child and adolescent psychiatrists are needed to meet the needs of children.
You Might also like
-
Streamlining and centralising training for gastroenterologists
Dr Amit Saha is a Paediatric Gastroenterologist and Hepatologist and trained paediatric endoscopist based in Perth. He underwent his higher specialist training in Paediatrics within the NHS in the UK, and sub-specialised in Paediatric Gastroenterology Hepatology & Nutrition at busy and prestigious centres in London including The Kings College Hospital.
-
Prioritising Oral Health in Aged Care and Disability Support
Leonie Short is a Dental Practitioner and Dental Therapist. She started working as a dental therapist in Rural NSW and then moved into being an academic and researcher. Through her career, Leonie has worked at 6 universities across New South Wales and Queensland, and remaining community focused.
Leonie’s mission is to have improved oral health experiences and outcomes, however she recognises, the health system really needs to work hard to make it happen and for people to understand why it needs to be a priority.
-
Australian Healthcare and Hospitals Association Hospitals and Clinics New Content Value-Based Health Care
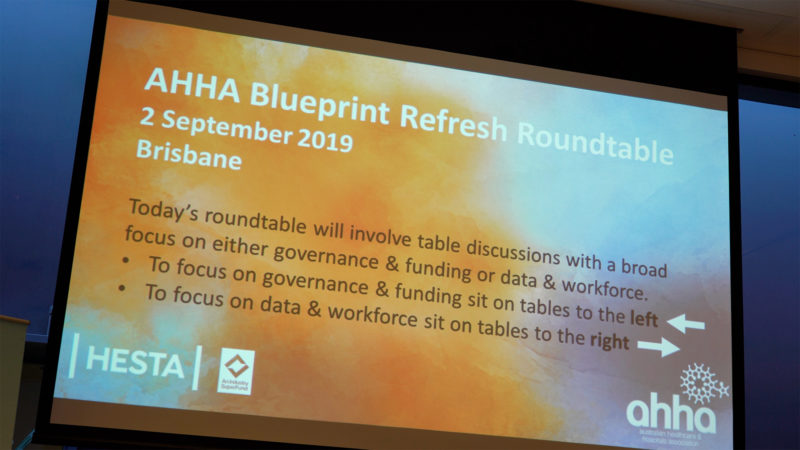
Australian Healthcare and Hospitals Association (AHHA) Blueprint Refresh Roundtable
AHHA’s Blueprint Refresh Roundtable brings together AHHA members and other Australian health leaders to evaluate the progress made to date against Healthy people, healthy systems and to tease out key policy issues that need to be addressed in order to implement outcomes-focused, value-based care in Australia.