According to a prominent paramedicine academic and researcher, paramedics have the potential to provide much-needed care in the community, changing the traditional healthcare model. Research points to paramedics having a wider healthcare workforce impact based on their ability to identify and fix problems 24/7.
Dr. Brendan Shannon is Head of Postgraduate Programs in the Department of Paramedicine at Monash University and a member of The Australasian College of Paramedicine. His interests including refining healthcare models, to ensure underserved communities receive requisite care. These alternative care pathways, like outreach programs, can work out of hospitals to provide care in underserved communities with social and complex chronic conditions.
Dr Shannon states, “Paramedics can be utilised in a proactive outreach manner, not just responding to emergency calls, to provide care to those who need it most. The role of paramedics needs to further evolve to see patients with chronic diseases so that they don’t end up in an emergency situation, rather than only responding to emergencies.”
Dr Shannon is a registered paramedic and academic innovating new education programs and paramedicine models of care and career pathways – including as the Education lead of the $20.3 million Australian-first Paramedic Practitioner Program being delivered by Monash University in partnership with Ambulance Victoria and Safer Care Victoria.
Australian Health Journal met with Dr Shannon to health about his research in alternative care pathways and community medicine, involving paramedic roles.
You Might also like
-
Mid-Career Nurse Leadership Program
How does a nurse navigate senior management to affect change within their organisation? It’s a gap that Australian College of Nursing is helping to fill with it’s Mid-Career Nurse Leadership Program that gives established nursing professional access to prominent leaders in nursing.
-
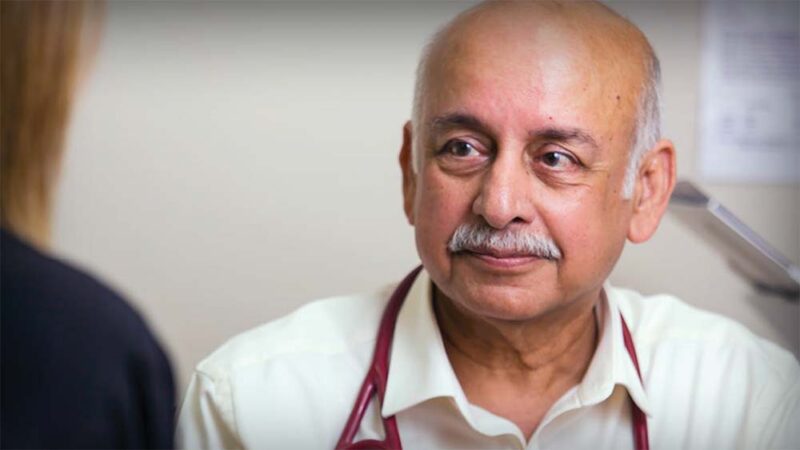
GP Health of The Nation
As Australia’s largest professional general practice organisation, the RACGP represents more than 43,000 members, including more than 24,000 Fellows who have completed specialist training (or its equivalent). These are the frontline GPs who treat almost 22 million patients across the country every year.
Each year the runs a survey across Australian Doctors. This year’s report reflects the experience of more than 1300 RACGP Fellows from across Australia. Despite this and other achievements, the share of total government healthcare spend for primary care is in decline.
-
Sharing the same goals in value-based procurement
Value-based procurement (VBP) is a journey, not a sprint. It’s about putting the patient at the centre of quality affordable healthcare through changes in procurement practices for medical technologies. Patient outcomes drive value and sustainability, not just price. The bigger picture indicates that VBP will create system cost saving through benefitting patients, rather than trying to attain the reverse – a win-win outcome.